
Is cannabis right for your dog or cat?
Dexter, Watson, Teekl, Rufus, Muffin, Buttercup, Angel face. Regardless of what you decide to call them, our pets are loved and an important part of our family. They deserve the best care, especially when it comes to treating and managing their chronic conditions. Conventional medications have proved useful, however, many come with a slew of unwanted side effects. Pet owners are continually searching for safer alternatives to improve the quality of life for their furry loved ones.
Cannabidiol (CBD) is a non-intoxicating phytocannabinoid abundant in the Cannabis Sativa L. plant. Its wide range of therapeutic uses and low toxicity profile make it a favourable choice to treat conditions such as anxiety, pain and seizure disorders. Although more studies are needed to determine dosing, long-term use and safety, CBD is becoming the go-to alternative to pharmaceutical medications.
Veterinarians are continually advocating for the use of cannabis-based products in animals. The Canadian Association of Veterinary Cannabinoid Medicine (CAVCM) is a prominent advocacy group pushing for access, research and education for cannabinoid therapy in animals. Both The Canadian Veterinary Medical Association (CVMA) and The American Veterinary Medical Association (AVMA) are in favor of expanding veterinarians as authorized medical prescribers[1] and “enthusiastically support[s] exploring the therapeutic potential of cannabis-derived products.[2]
Fear and anxiety are normal emotions for all animals. It is known as the ‘fight or flight’ response, protecting animals in stressful situations. However, if the body is unable to restore normal functionality, this emotional stress can lead to anxiety disorders and thus have a negative impact on the animal’s health and wellbeing. Approximately 20%[3] of dogs experience some form anxiety presenting as:
First line treatment is conditioning and desensitization. If these methods fail, medications are prescribed. Common medications to treat anxiety include:
These prescribed medications, although well studied, may come with side effects such as sedation, diarrhea, insomnia, behavioral changes, and itching.

Chronic pain affects approximately 30% of the pet population, mainly affecting older dogs and cats.[5]
Left untreated, pain can reduce the quality of life and lead to comorbid conditions such as anxiety, fear, depression and anger. Chronic pain can present as:
There are many human medications that are formulated for pets. Common treatments for pain include:
These treatments have been shown to alleviate pain, however they come with a list of side effects that may affect the quality of life (QoL) of the pet. In a systematic review of 29 clinical trials, 55% of dogs treated with NSAIDs observed gastrointestinal side effects such as diarrhea and bleeding.[6] Other side effects can include sedation, weight gain, itching and restlessness.

Mammals, fish, birds, amphibians, sea urchins, molluscs and leeches possess an endocannabinoid system (ECS).[7] This is a protective signaling system and it is vital to our health and normal physiologic functions. If we encounter chronic conditions such as pain, seizures, anxiety and depression, our ECS is overworked, resulting in a clinical endocannabinoid deficiency. Cannabinoids such as CBD are administered to restore this imbalance.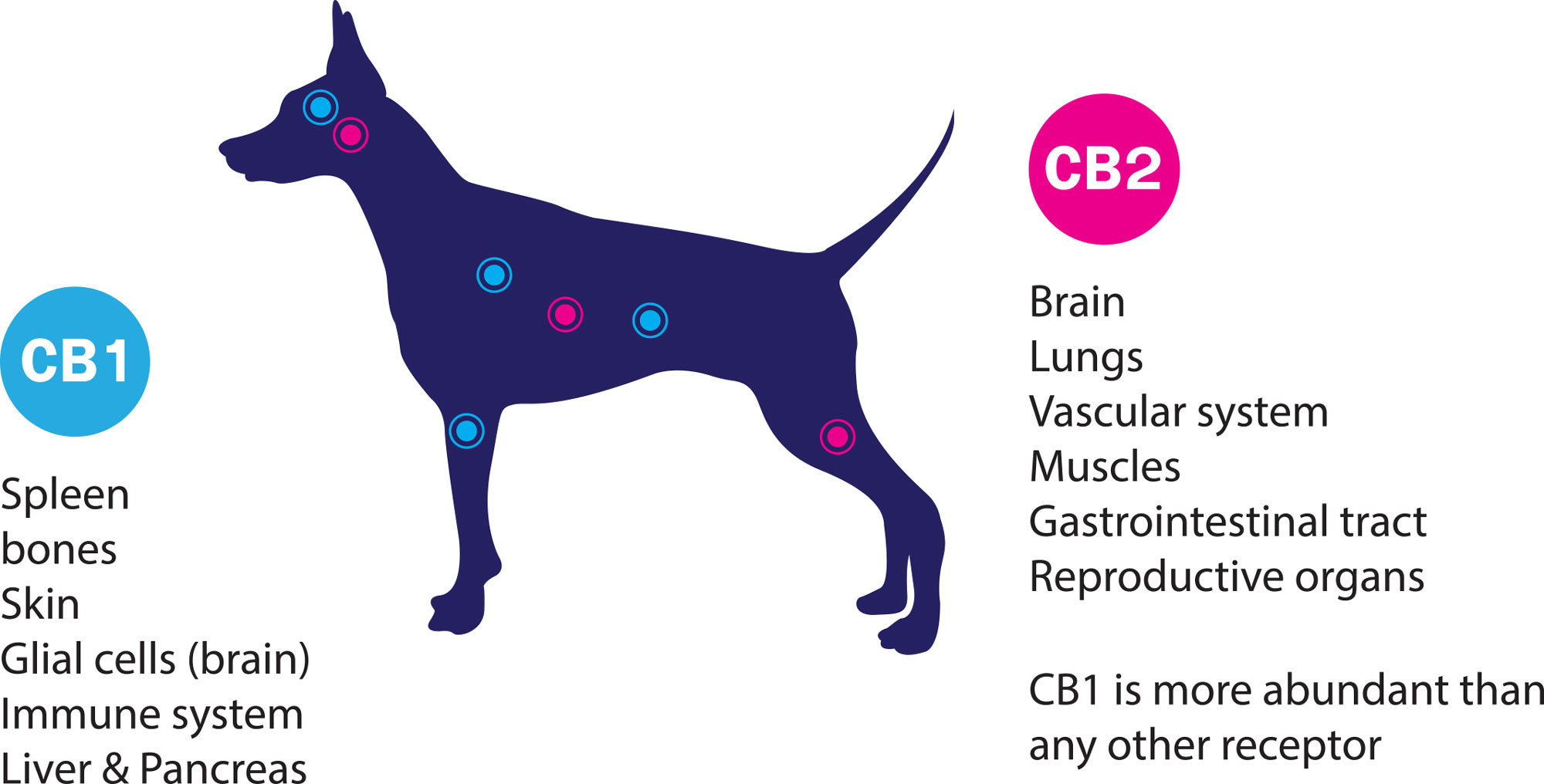
The endocannabinoid system is involved with regulation of homeostasis. In times of stress aka excitotoxicity, the ECS is activated to protect and restore proper functionality. When studied in mice, the levels of 2-AG, an endogenous cannabinoid, are significantly increased after injury, suggesting a protective mechanism to reduce inflammation, modulate neurotransmitter release and improve recovery[8]. Increases in intracellular calcium also trigger the release of endocannabinoids, 2-arachidonoyl-glyercol (2-AG) and anandamide (AEA), which serves to block calcium channels and reduce further damage.
Unfortunately, there are very few studies examining the safety and efficacy of CBD in small animals. In a 2018 randomized controlled trial[9], CBD was shown to have efficacy and safety in osteoarthritic dogs. The researchers took 16 dogs and compared a 2mg/kg full spectrum CBD in olive oil containing 0.25mg THC/ 10mg CBD per 1 ml versus placebo, dosed every 12 hours. The outcomes of the trial showed that CBD significantly reduced pain and increased activity with no significant adverse effects.
Dosage varies depending on weight and condition. The best approach is to:
The trial mentioned above utilized a 2mg/kg dose.
CBD is generally well tolerated with minimal toxicity. In a study conducted by Colorado State University[10], 30 dogs were given CBD at varying concentrations for 6-week trial period. The most notable side effects observed were:
Dosage varies depending on weight and condition. The best approach is to start at a low dose (0.5mg/kg) and titrate every 2-3 days until symptoms resolve or side effects appear. The trial mentioned above utilized a 2mg/kg dose.

Pets are curious and sometimes eat things they aren’t supposed to. There have been numerous reports of dogs ingesting cannabis or edible products such as brownies or cookies. In fact, in areas of the United States that have legalized cannabis, the Pet Poison Helpline has seen a 448% increase of cannabis ingestion cases.[11] If you think your pet has ingested cannabis, look out for signs and symptoms[12] of cannabis toxicity:
If you suspect your pet has ingested cannabis, it is recommended to take them to your veterinarian or nearest animal hospital. Most ingestions are self-limiting, and symptoms can dissipate within 12 hours. Below are some tips to help your pet during this time:

It is always important that if you are consuming cannabis for recreational or medical purposes, that you store your cannabis away from pets and children. Purchase a good lockbox and store your cannabis in high cupboards that are out of sight for vulnerable populations.
Although we have been using cannabis for millennia, the medicinal use of cannabis in animals is still in its infancy. More research is necessary to determine dosing guidelines, drug interactions and examine the adverse effects of cannabis. Cannabis has shown a tremendous amount of promise in the treatment and management of various medical conditions. For more information on Cannabis and Pets please visit the following resources or contact us at The Pharm.